Originally published Winter Newsletter 2024. Written by Deb Cooke, PA-C.
Precepting a student seems like a challenge in an already strained system. Often, we feel there is not enough time, our patients are too difficult, or we worry we aren’t a good teacher. On top of it, we undoubtedly feel some level of burnout and struggle to get through our week. Keeping all of this in mind, I still think you will make a great preceptor! Hear me out:
There’s not much extra you need to do when you have a student! Of course they will be asking some questions, and you will likely have to hear oral presentations that bring you back to your own rookie year, but these won’t take too much time. Ways to help you, the preceptor, navigate these:
Have your student take time to prepare their oral ahead of time. Let them use notes if helps speed things up. Let them present the patient the next week if they need more practice. Make sure they highlight things that are pertinent to the case so they learn to triage info and trim time. The sooner they understand “pertinent positive and pertinent negatives” the quicker they will get to quality oral presentations.
Let them do their own research on their questions. If the answer to their question is too vast, tell them to research it on their time and they can discuss it with you in their next session. Part of their learning is to find out information through many sources. Have them tell you the next session what they discovered and if they have questions at that point.
Let them just follow you for a bit. Students of today have grown up in a world of messaging to communicate and often struggle with real-time live communication with non-peers. With you, students can watch you interact with patients as they will need to in the future. They will be able to model all the soft skills of interpersonal relationships. I can’t stress enough how important it is for students to learn to speak with patients and handle the nuances of information clarification, sensitive conversations and showing empathy.
Use your typical time constraints with patients to mimic the efficiency needed with your time with the student. Although you have agreed to take on a student, you still have a job to do. Let them know they are also going to be part of the quicker tempo. Let them know up front that there will be sometimes when you can have a longer conversation and sometimes when you need to move things along. If there happens to be opportunities to allow them more time with a patient, they can take it but it should not be an expectation. The pressure of building rapport and gathering patient information as well as a physical exam is part of their learning as well.
Have students reflect on non-scientific things they learned each day. We remember that PA school was overwhelming and students often move onto the next task in their mountain of tasks. But the patient encounter carries so much more than medical information. So many of our health care challenges surface during the patient interaction. Chances for humanity, respect, insurance issues and barriers to care will emerge and offer learning opportunities. Having some time for self-reflection will enhance their experience and highlight the often overlooked teaching moments. Time with you will offer so many valuable moments they would not get otherwise.
Keep things simple. Students have lot of random information in their brains, mnemonics for days, and a realization they have no idea what they are doing with it! Allow them to see the information as it relates to the big picture. Bring concepts back to “sick vs not sick”, “stable vs unstable”, “acute vs chronic” etc. Sometimes stepping back to big picture helps students understand the patient treatment. It’s easy to get lost in the details so help guide them out.
Ultimately these students are learning how to become a good PA. Skills they will learn with you will go well beyond knowledge. They will be grateful for the experience and will remember the time with you for most of their careers. And… you can earn category 2 CME credit for every hour you precept (up to 50)!
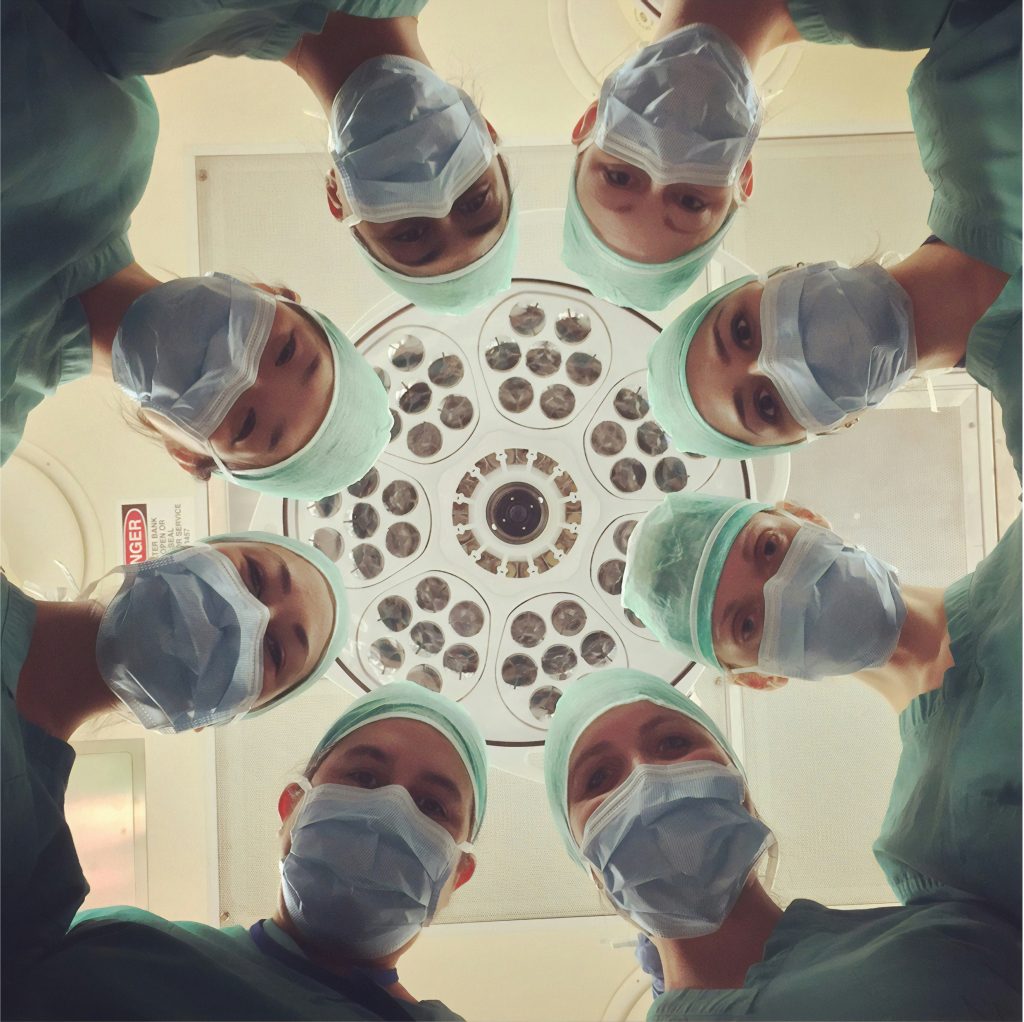
Photo Credit: Photo by National Cancer Institute on Unsplash